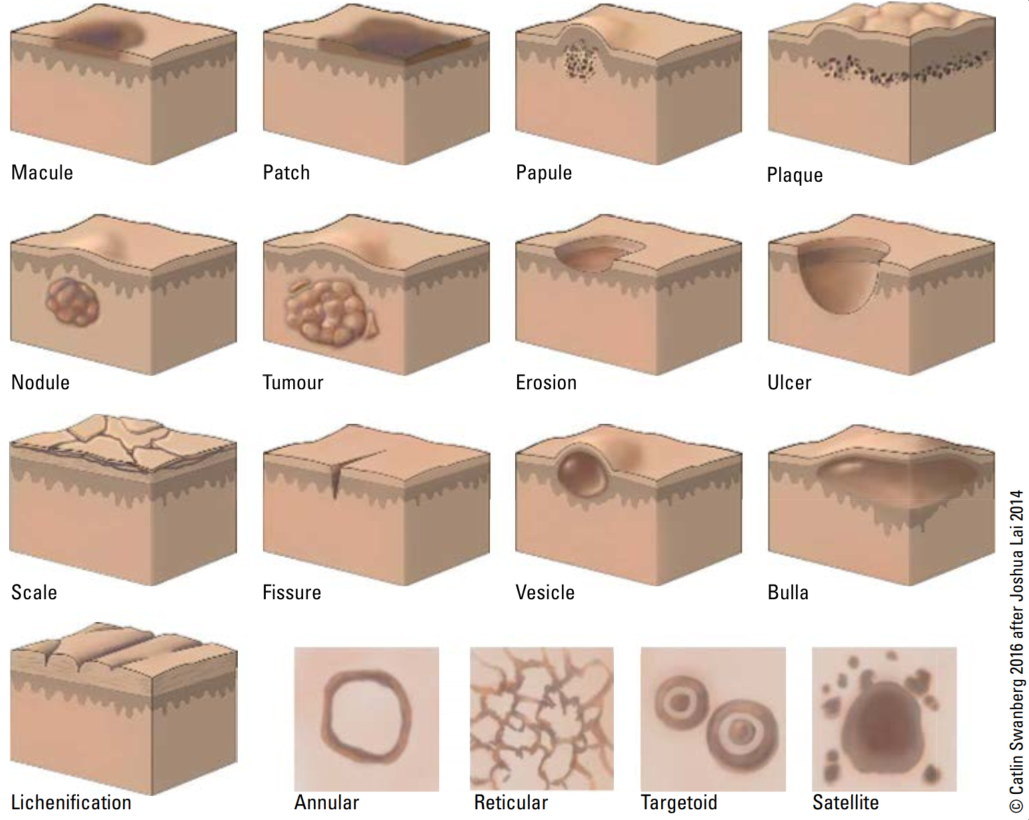
Describing lesions
Primary lesion: de-novo un-altered lesion Secondary lesion: evolution of 1' lesion
Basic lesion descriptors
| Profile | <1cm diameter | >1cm diameter |
|---|---|---|
| Flat | Macule | Patch |
| Raised superficial | Papule | Plaque |
| Deep palpable | Nodule | Tumor |
| Fluid filled | Vesicle | Bulla |
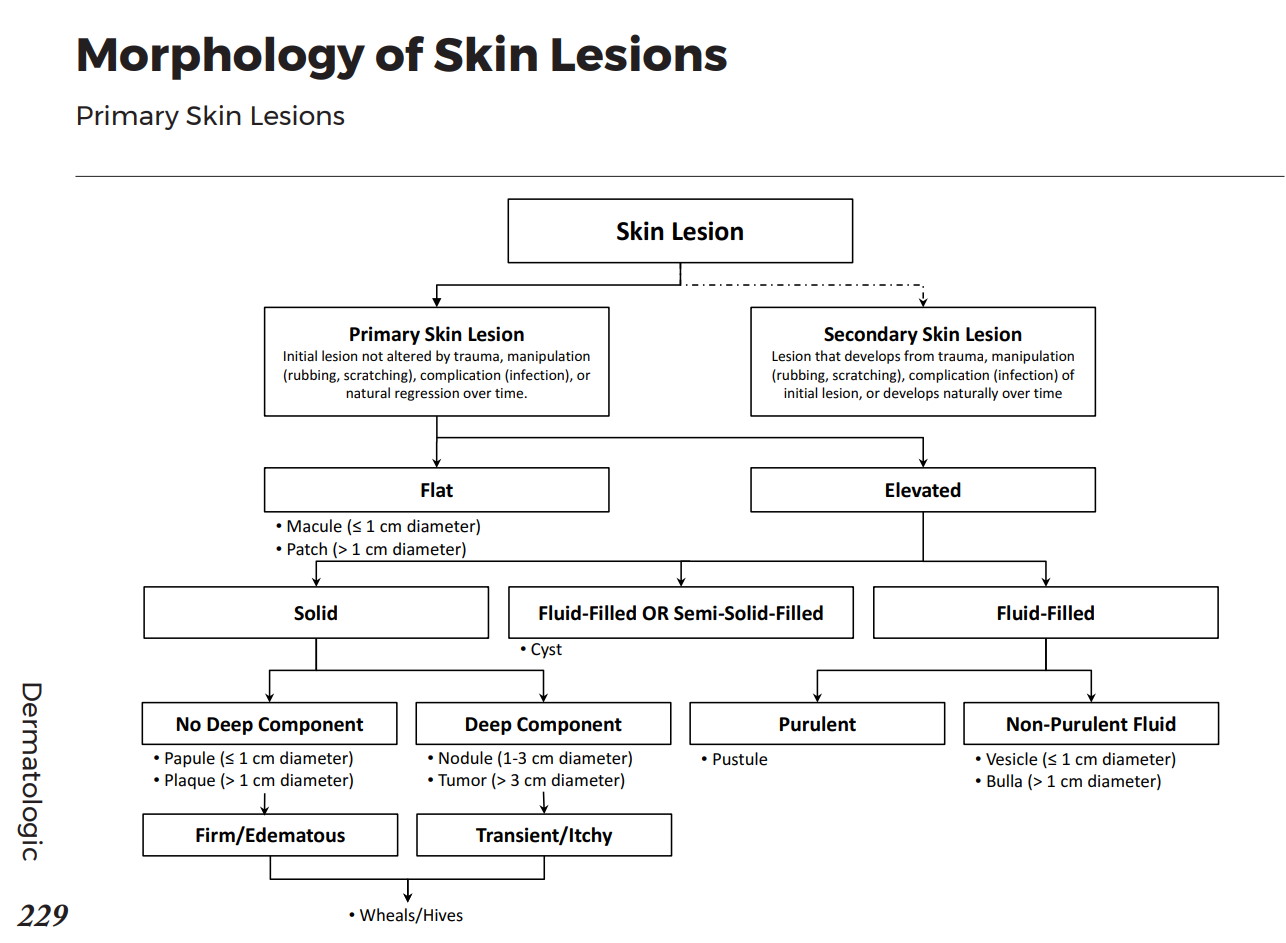
Other lesion nomenclature
Pattern nomenclature
Approach to skin lesions
Lesion History
- Onset
- Location
- Pattern of spread
- Evolution
- Provoking factors (ie heat, cold, sun, exercise, travel, medications, pregnancy, season
- Associated symptoms (ie pain, itch)
Associated symptoms
- Acute: headache, chills, fever, weakness, night sweats
- Chronic: fatigue, weakness, anorexia, weight loss
Other particular things on consult history
- PMHx any skin conditions, chronic diseases, etc; FHx of psoriasis, atopy, melanoma, etc; Social history focus on travel and chemical exposures, home environment, sick contacts; Meds, don't forget OTC
Diagnosis
Often hinges on history and physical exam. Frequently however, biopsy may be done to confirm or establish a diagnosis.
HISTORY PEARL
Remember SCALDA to describe a lesion:- S - Size/Shape/texture
- C - Colour
- A - Arrangement
- L - Lesion type - primary vs secondary
- D - Distribution - ie Symmetrical, dermatomal, follicular, extensor surfaces, intertriginous (between body folds), dependent areas, sun-exposed skin
- A - Always check condition/involvement of mucous membranes, nails, hair, and intertriginous areas
Common treatments
Topical steroids
| Potency | Relative Strength | Generics | Brand | Usage |
|---|---|---|---|---|
| Weak | x1 | hydrocortisone–2.5% (1% and 0.5% available over-the-counter) | Emo cort | Intertriginous areas, children, face, thin skin |
| Moderate | x3 | betamethasone-valerate-0.1%; hydrocortisone 17-valerate-0.2%; desonide; mometasone furoate | Betaderm; Hydroval; Tridesilon; Elocom | Arm, leg, trunk |
| Potent | x6 | amcinonide | Cyclocort | Body |
| Very potent | x9 | betamethasone dipropionate-0.05%; fluocinonide-0.05%; halcinonide | Diprosone; Lindex; Lyderm; Halog | Palms and soles |
| Extreme | x12 | Clobetasol propionate-0.05% (most potent); betamethasone-dipropionate ointment; halobetasol proprionate-0.05% | Dermovate; diprolene; ultravate | Palms and soles |
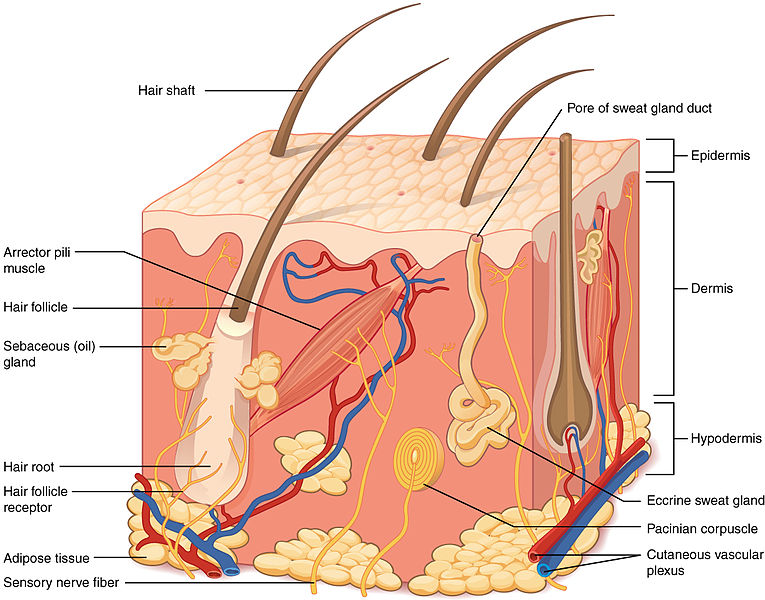
PHSYIOLOGY
Skin functions:
- Protection: continuous recycling and avascularity of epidermis; barrier to UV radiation (melanin), mechanical/chemical insults (sensory/mechanoreceptors), pathogens (immune cells, bactericidal chemicals in sebum, acidic sweat), and dehydration (lipid rich barrier)
- Thermal Regulation: insulation to maintain body temperature in cool environments; dissipation of heat in warm environments via sweat glands and increased blood flow
- Sensation: touch, pain, temperature
- Metabolic: vitamin D synthesis, energy storage of adipose tissue
- Excretion and absorption: Loss of fluid through sweat, carbon dioxide. Small absorption of lipid-soluble materials (ie gases, steroids, KADE, some toxins).
Skin Flora
- Skin microflora is dominated by staphylococci (especially coagulase-negative staphylococci, which are a collection of different organisms), streptococci (B hemolytic, especially), corynebacteria, and propionibacterium.
- Skin near the perineum and rectal region tends to have more enteric organisms present, such as enterobacteriaceae, enterococci, and bacteroides species.
- Keratinocytes and other constituents of skin prevent colonization by other (relatively pathogenic) organisms; when skin is unhealthy, they are prone to colonization by pathogenic organisms (such as S. aureus in patients with psoriasis).
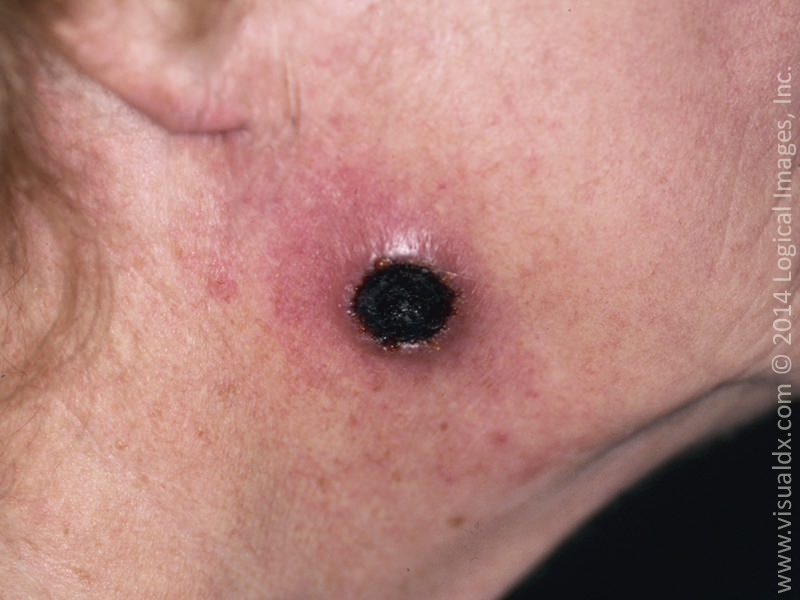
Resources / Image References
- LearnDerm by visualdx is an amazing resource for fundemental dermatology and has an excellent collection of photos. Click HERE to see more.
- American Family Physician: 1) Generalized Rash DDx 2) Generalized Rash Approach 3) Derm Emergencies 4) Index of other articles
- DermNet NZ is a free wiki with lots of pictures about many conditions. https://dermnetnz.org/
- https://canadiem.org/describing-a-rash/
- Toronto Notes 2020
- American Academy of Dermatology
- UBC's pediatric guide to skin lesions